This "dog" is a true omnivore, not unlike homo sapiens. It supplements a diet of meat (frogs, fish, lizards and other small game) with fruit, tubers, and sugarcane. These supply up to 51% of its diet. It does not do well in captivity without vegetable foods, In the wild it is susceptible to infestation by the Giant Kidney Worm (Dioctophyme renale), a potentially lethal roundworm it is exposed to by eating fish. It prefers the fruit of the Wolf Apple (Solanum lycocarpum) or lobeira, a tomato like fruit (also related to the Goji or Wolfberry) which is believed to protect it against this parasite (1).
Cindy Engel writes in Wild Health (a 2002 book which is recommended reading for anyone interested in Ancestral Health):
"Although this fruit is more plentiful in certain seasons, the wolf works hard to eat a certain amount throughout the year... researchers at the Brasilia zoo found that when packs of captive wolves were fed lobeira daily, they survived. If lobeira was withheld, all the wolves died. Postmortem examinations revealed giant kidney worm infestations, and it was suspected that lobeira might be controlling these worms in the surviving wolves".
The Maned Wolf also seems unusually susceptible to cancers in captivity (2)
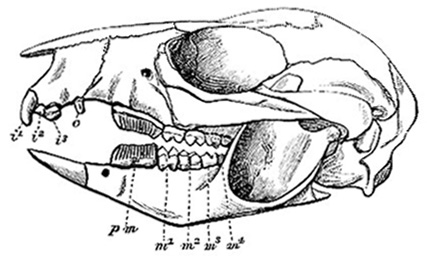
Whether or not the maned wolf is self-medicating, we can learn a lot by looking at its teeth:

Teeth adapted, as the Maned Wolf is, to a diet that can be 51% plant based.
Let us compare that with the dentition of Homo Sapiens, a creature adapted to eating a diet similar to that of the Maned Wolf, with, on average, a broadly similar split between animal and plant foods:

We can clearly see that the dentition of a species need not be specific for its adapted diet. The Maned Wolf finds animals hard to catch and kill; it is not going to lose its carnivorous dentition because it eats fruit (although too much indulgence in the sugar cane could conceivably have that effect in individuals). The ancestral savannah-dwelling hominid, perhaps a former insectivore and fruitarian, finding itself "tuskless in Eden" in Robert Ardrey's evocative words from African Genesis, survived by developing tools that do the work the Maned Wolf's incisors do. Humans have not needed to trade away teeth that are useful for gripping the ends of the cords used to tie spearheads onto shafts, as well as for crushing seeds and roots. We can chop and stab and saw where the Maned Wolf can only tug and gnaw. The leg joints of quadraped mammalian carnivores are well designed for maximum force in tugging as well as speed in leaping and running.
Man is neither of these things (below), but it's fair to say that for quite a few aeons now he has had more in common with the dog than with the sheep. Especially if that dog is the Maned Wolf.

For comparison, the dentition of a Kangaroo, a marsupial herbivore which has evolved separately from the sheep:
This is the Maned Wolf's closest living relative, the Bush Dog, in flagrante delicto. This tough and gregarious 5-8 Kg canid can hunt the 40 Kg peccary, and a pack has been seen hunting a 250 Kg tapir.
It seems to be a wholly carnivorous creature.

The legs of the Bush Dog are adapted for strength in tugging at its larger prey, whereas those of the Maned Wolf are more suited for leaping on the small, swift creatures that make up its animal diet.