I remember this passage, from Iris Murdoch's "The Flight from the Enchanter", every day, and especially when I receive information that may cause me to modify my hypothesis.
Reading up on cholesterol with regard to Dr Yu's study that I discussed in my last post (a study of chronic hepatitis C cases, non-responders, showing increased progression of fibrosis and cirrhosis with higher cholesterol intakes), it becomes quite obvious that cholesterol should have a role in fibrosis and cirrhosis.
Apt tune; Rufus Wainright, Cigarettes and Chocolate Milk
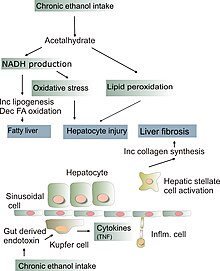
You can cause fatty liver in an animal with a variety of strategies; a methionine-choline deficient diet, alcohol plus linoleic acid, a high fat diet (unless the fat is butter or coconut oil, or the animal is intermittently fasted); or fructose plus linoleic acid. The latter two are models of NAFLD (non-alcoholic fatty liver disease). NAFLD can progress to NASH, non-alcoholic steatohepatitis, an inflammatory disease which results in fibrosis and cirrhosis.
What is needed to turn NAFLD into NASH in rodents? Dietary cholesterol. 1% (which is a lot).
What happens if cholesterol is added to the alcohol-linoleic acid (or indeed fish oil) model of alcoholic liver disease?
In rats given intragastric ethanol and either corn or fish oil,
addition of cholesterol (1%) does not change the degree of
fatty infiltration but prevents hepatic necrosis and inflammation
and enhances hepatic fibrosis. Cholesterol in this model
decreases the enhanced low-density lipoprotein receptor
message, eliminates messages for TNF-a and COX-2, and
decreases plasma and liver levels of thromboxane B2, and
products of lipid peroxidation, whereas it increases transforming
growth factor-b message. The anti-inflammatory effects of
cholesterol are most likely related to a decreased uptake of
arachidonic acid caused by downregulation of the low density
lipoprotein receptor and its decreased conversion to
eicosanoids via decreased COX-2 activity. Enhanced fibrosis
may be mediated by increased transforming growth factor-b.
(TGF-beta being a signal that activates hepatic stellate cells).
What happens in a non-alcohol model?
Livers of DD-fed mice showed histological changes resembling NAFLD, including steatosis and modest fibrotic changes; however, DDC-fed animals developed micro- and macrovesicular steatosis, inflammatory cell foci, and fibrosis resembling human NASH. Dietary cholesterol also exacerbated hepatic macrophage infiltration, apoptosis, and oxidative stress.
Dietary cholesterol appears to confer a second “hit” that results in a distinct hepatic phenotype characterized by increased inflammation and oxidative stress.
What sorts of factors that set the stage for a NASH-like syndrome might be present in HCV patients?
(Note that HCV fibrosis differs from NASH in that it is spread more evenly through the liver, consistent perhaps with an intracellular causative agent).
The NAFLD diet above is described as "diabetogenic", and NAFLD is associated with diabetes, obesity, and metabolic syndrome. The animal diets that cause it and predispose to NASH require the same nutrients that, frankly, cause diabetes and NAFLD in humans. Seed oils, lard, and refined carbohydrates that are predominantly sugar (also fish oil, but only in doses that no-one ever ate). Round the clock feeding and overfeeding. Factor in HCV, which is diabetogenic in its own way and (Genotype 3) promotes steatosis (incidentally, Genotype 3 does the most to depress cholesterol completion, and would logically benefit most from dietary cholesterol were the NASH issue moot).
Another point that might be of major importance to humans is the n-6:n-3 ratio.
Introduction and aim: Essential dietary polyunsaturated fatty acids (PUFA) include omega-6 (n-6) linoleic acid (18:2) which is metabolized to arachidonic acid (AA) and omega-3 (n-3) linolenic acid (18:3) which is metabolized to eicosapentanoic acid (EPA). Imbalance in secondary eicosanoids and prostaglandin metabolites of n-6 and n-3 PUFA are implicated in disorders related to the metabolic syndrome. Skeletal muscle PUFA influences systemic insulin sensitivity (Borkman 1993) and diets rich in omega-3 fatty acids are associated with diminished histological injury in NASH (Musso 2003). Erythrocyte membrane lipids reflect dietary intake of essential fatty acid over preceding months. We measured erythrocyte n-6:n-3 ratio in a cohort of patients as part of a larger study of omega-3 fatty acid therapy of NASH.
Methods: 15 patients (10 female) underwent analysis of erythrocyte lipid composition using capillary gas chromatography (Metametrix, Duluth, GA) to determine the AA:EPA ratio. The mean age was 50 ± 13 years all with liver biopsy NAS score ≥ 5 and a range of non-cirrhotic fibrosis stages of stage 1 (n = 6), stage 2 (n = 5) and stage 3 (n = 4).
Results: The mean AA:EPA was 65 ± 34 reflecting a relative excess of n-6 PUFA overall. However, a broad range was noted from 15 to 144 AA:EPA. Dividing the group into quintiles of the reference range, 9 of the patients fell into the highest (5th) quintile (AA:EPA = 84 ± 30) compared to the remaining 6 patients (AA:EPA = 36 ± 16, p = 0.001). There was no statistically significant difference in the histological stage between these groups (fibrosis score = 2 ± 0.9 versus 1.7 ± 0.8) although the higher AA:EPA group was significantly older (55±12 versus 39±12, p=0.01).
Conclusion: There is heterogeneity of AA:EPA in non-cirrhotic NASH patients and an age-related increase in n-6 to n-3 PUFA evident in the AA:EPA ratio of erythrocyte lipids. Further work is needed to understand if this reflects dietary differences and how this might influence response to omega-3 fatty acid therapy.
There is a 2012 review of Omega-3 interventions in NAFLD/NASH here.
If I might digress for a moment, I came across 2 very interesting epidemiological papers about age-related macular degeneration (AMD). Both identified linoleic acid as a factor promoting the disease, and a protective effect of fish oil and fatty fish - but this protective effect was only seen in those subjects with the lowest intake of linoleic acid:
Higher intake of specific types of fat--including vegetable, monounsaturated, and polyunsaturated fats and linoleic acid--rather than total fat intake may be associated with a greater risk for advanced AMD. Diets high in omega-3 fatty acids and fish were inversely associated with risk for AMD when intake of linoleic acid was low. Conversely, neither omega-3 fatty acids nor fish intake were related to risk for AMD among people with high levels of linoleic acid intake.
Note that this first paper distinguished between vegetable and animal fats and only found a harmful association with vegetable fats. The second paper combined all fats:
Saturated, monounsaturated, polyunsaturated, and transunsaturated fats increased the likelihood of progression (RR, 2.09 and P trend =.08; RR, 2.21 and P trend =.04; RR, 2.28 and P trend =.04; RR, 2.39 and P trend =.008, respectively). Higher fish intake was associated with a lower risk of AMD progression among subjects with lower linoleic acid intake. Processed baked goods, which are higher in some of these fats, increased the rate of AMD progression approximately 2-fold, and nuts were protective.
Note that nuts were protective against a linoleic acid mediated disease. I hope the significance of that is not lost on you!
Well here we have someone eating a standard western diet, lots of refined starches, sugars and omega 6 oils.
They decide to throw in a bit of cholesterol, say a bacon burger and an egg McMuffin, and their NAFLD is more likely to turn to NASH.
What about people with chronic HCV infection?
Am J Gastroenterol. 2005 May;100(5):1091-8.
Factors associated with the presence of nonalcoholic steatohepatitis in patients with chronic hepatitis C.
Solis-Herruzo JA, Pérez-Carreras M, Rivas E, Fernández-Vázquez I, Garfia C, Bernardos E, Castellano G, Colina F.
Source
Departments of Gastroenterology and Pathology, Hospital Universitario Doce de Octubre, Madrid, Spain.
Abstract
OBJECTIVES:
The aim of this study was to identify factors associated with the presence of nonalcoholic steatohepatitis (NASH) in patients with chronic hepatitis C (CHC).
METHODS:
We studied 98 patients with CHC [47 with NASH (group HCV/NASH), 51 without NASH (group HCV)] and 85 with NASH not infected with hepatitis C virus (HCV) (group NASH). We determined factors associated with the presence of NASH in patients with hepatitis C.
RESULTS:
Group HCV/NASH patients resembled those with NASH. Body mass index (BMI) was higher in group HCV/NASH than in group HCV, but was similar to group NASH. Most HCV/NASH patients had risk factors for NASH. In patients infected with HCV, NASH and NASH-related lesions were independently associated with BMI, while steatosis score was associated with HCV genotype 3 and BMI. Fibrosis stage was independently associated with steatosis, necroinflammatory activity index, and NASH lesions.
CONCLUSION:
While HCV genotype 3 infection and BMI are associated with the presence of steatosis in CHC, BMI is the only factor independently associated with the presence of NASH in these patients. We suggest that overweight-related factors might induce NASH in CHC patients.
When Ned Kock re-analysed the Bridges data he came to this conclusion:
What the results summarized in this post do suggest is that pork consumption may not be a problem at all, unless you become obese from eating it. How do you get obese from eating pork? Eating it together with industrial foods that are addictive would probably help.
What the results summarized in this post do suggest is that pork consumption may not be a problem at all, unless you become obese from eating it. How do you get obese from eating pork? Eating it together with industrial foods that are addictive would probably help.
It looks like Ned was right, after all.
It's worth remembering what Bridges, Nanji and French did with the pork data. They didn't make a big case of it in the media and try to demonize pork. Instead they hypothesized about causes and developed animal models for testing the role of PUFAs in alcoholic liver disease. The result is the body of research that tells us - with a clarity that is unusual in diet-health science - that high-PUFA diets promote alcoholic liver disease, and highly saturated fats protect against it. French summarizes his conclusions here in a response to a paper by Amin A. Nanji called "Dietary saturated fatty acids: a novel treatment for alcoholic liver disease".
French indicates that more than 1.5% calories from PUFA will promote liver damage while an alcoholic is drinking (at least at a standard 35% fat diet), while the use of lecithin (or presumably fish oil) may be safe during recovery.
In summary, any therapeutic trial for the treatment
of ALD should be predicated on a rationale based on
experimentally shown efficacy. Using such guidelines,
the use of the feeding of dietary fats, such as palm oil,
other fats low in polyunsaturated fatty acids, or linoleic
acid, should benefit patients with ALD in the alcoholic
withdrawal phase of alcoholic hepatitis. However, to pre-
vent further liver damage during periods of alcohol abuse,
fats that contain substantial linoleic acid or polyunsatu-
rated fats should be avoided. This is because any fat
ingested that provides more than 1.5 % of dietary calories
may permit liver damage induced by alcohol to be mani-
fested. At least this is true in the growing male rat that
is fed ethanol by intragastric tube. Palm oil used by
Nanji et al. contained 8% linoleic acid, which in the
case of the rat model of ALD would not be expected to
protect the liver from injury when ethanol is ingested.
Likewise, this would also be true if patients with ALD
were treated with soybean lecithin supplements if they
continued to drink because soybean lecithin is very rich
in linoleic acid. Of course, there is a danger in extrapo-
lating animal data to humans. For instance, a diet rich
in saturated fat may have negative side effects such as
worsening cardiovascular disease in humans. Because of
this potential danger, caution should be exercised if the
animal data are to be used as rationales for the treatment
of patients with alcoholic hepatitis.
Well, thank goodness we don't need to worry about that any more.
So to summarize, high levels of cholesterol in the diet may be harmful to persons with fatty liver disease, especially in persons with chronic HCV and high BMI, unless they are in a diet designed to clear a fatty liver.
Even then, there may well may be a brief transition period in which it may be wise to limit cholesterol. Exactly how much, I haven't a clue.
Even then, there may well may be a brief transition period in which it may be wise to limit cholesterol. Exactly how much, I haven't a clue.
6 comments:
Two afterthoughts -
1) there may indeed be a benefit in limiting cholesterol at some points when trying to reverse fibrosis or treat cirrhosis. Probably not necessary if you are reversing fatty liver, and may be protective in acute toxic hepatitis. What I have in mind at this stage is alternate days of cholesterol-rich foods (which are the most nourishing in terms of the likely deficiencies) then low-cholesterol fats such as cocoa, coconut, olive oil, nuts. But I'll think about this some more.
2) what Ned Kock said; it can not be just obesity that is the risk factor for cirrhosis, but factors associated with obesity (even in the thin) - type 2 diabetes, insulin resistance, a diabetogenic diet, metabolic syndrome, and so on.
Dear George,
a bit off thread , but, this paper which just came in, made me ponder about the role of external environments which is removed using mouse houses in research establishments. We have mild cold here now in Melbourne.
http://www.cell.com/cell-metabolism/abstract/S1550-4131%2813%2900247-7#Discussion
john
That is indeed interesting as just today I read a hypothesis that vasodilation (niacin and exercise were the example, but others would be UV light, antioxidants) was the protective factor against atherosclerosis.
http://tiny.cc/g2dozw
That would apply to cold environments, which are also more likely to be smoky/smoggy ones.
Of course eskimos were immune to heart disease, but did have atherosclerosis. Probably due to fires. Small animals need extreme strategies to survive cold.
I wonder if there is correlation between chillblains and CVF risk?
CVD, that is.
Sensational blog soundtrack selection, George. I'm enjoying catching up on posts now I'm back from Turkey. Riveting and thought-provoking material, as always.
Post a Comment