The title is:
Long‐term health effects of the three major diets under self‐management with advice, yields high adherence and equal weight loss, but very different long‐term cardiovascular health effects as measured by myocardial perfusion imaging and specific markers of inflammatory coronary artery disease.
The paper is published in Clinical Cardiology [edit: not Preventive Cardiology], and is free to access.
https://onlinelibrary.wiley.com/doi/abs/10.1002/clc.23047
[update: the paper above has since been retracted. Its Pubpeer discussion is here
https://pubpeer.com/publications/AA81ABA153565C2A238B191DFE0FB6 ]
[Update: the paper has been quickly republished here, in what may well be a predatory journal https://biomedres.us/pdfs/BJSTR.MS.ID.002006.pdf
Retraction Watch story here: https://retractionwatch.com/2018/11/13/a-convicted-felon-writes-a-paper-on-hotly-debated-diets-what-could-go-wrong/ ]
Three of the authors work at Fleming's medical imaging company in California, one is a deceased psychologist from Iowa, another is a pediatric nutritionist from New York and one is a Kellogg's employee from Illinois.
How this group was able to run a 12-month diet trial in 120 subjects is something of a mystery.
The conclusions:
One‐year body mass changes did not differ by diet (P .999). Effect sizes (R, R2) were statistically significant for all indices. Coronary blood flow, R (CI 95%) = .48 to .69, improved with low‐to‐moderate‐fat and declined with lowered carbohydrate diets. Inflammatory factor Interleukin‐6 (R = .51 to .71) increased with lowered carbohydrate and decreased with low‐to‐moderate‐fat diets.
Conclusions
One‐year lowered‐carbohydrate diet significantly increases cardiovascular risks, while a low‐to‐moderate‐fat diet significantly reduces cardiovascular risk factors. Vegan diets were intermediate.
First I'll consider all the good reasons to reject this study, but after that I'll do something we should always do, even for the worst study - take it at face value.
1) Lead author Dr Richard M. Fleming is a self-confessed and convicted felony fraudster who has admitted falsifying data in another RCT.
Fleming admitted to knowingly executing and attempting to execute a scheme to defraud Medicare and Medicaid healthcare benefit programs in connection with the delivery of and payment for healthcare benefits, items, and services, namely by submitting payment claims for tomographic myocardial perfusion imaging studies that he did not actually perform. Fleming also pled guilty to one count of felony mail fraud in violation of 18 U.S.C. 1341 and 2 for conduct relating to money paid him to conduct a clinical study of a soy chip food product for the purpose of evaluating health benefits. As Fleming admitted during his guilty plea, he received approximately $35,000 for conducting a clinical trial, but he fabricated data for certain subjects.https://www.federalregister.gov/documents/2018/09/28/2018-21210/richard-m-fleming-denial-of-hearing-final-debarment-order
2) Fleming obtained Robert Atkins' medical records by deception and shared them with Neal Barnard of the vegan activist group PCRM in 2004, another unethical behaviour and one demonstrating that Fleming has a long-standing animus against Atkins and his diet.
https://theskepticalcardiologist.com/2016/12/18/what-does-the-death-of-robert-atkins-tell-us-about-the-atkins-diet/
Now, vegans can do research into this exact question with a high standard of rigour, see Chris Gardner's studies - one can certainly dispute the interpretation of some results, but not the results themselves. And I have reviewed a vegan diet study favourably here (dealing with another Fleming paper in passing) - good results are good results; I don't doubt these diets can have also cardiovascular benefits over the short-to-medium term, but question their long-term effects on mental health, reproductive health, dental health, joint health etc.
3) The trial protocol number on the paper links to a study that was completed in 2002. This explains how a convicted felony fraudster was able to conduct a study. The protocol was posted in 2006, 4 years after the study concluded, which seems unusual on the Clinical Trials website.
https://clinicaltrials.gov/ct2/show/NCT00324545
4) The study has 35 citations - 15 of these are to Fleming's own papers. This self-spamming, which helps boost an author's citation rate, is frowned upon by reputable journals. One of these references has the word "quantum" in the title. Other references are to news articles and book chapters. The low carbohydrate diet references are more than 15 years old. Ref 16 is curious as an anonymous reviewer is given credit for the wording of a paragraph of interpretation, surely a run-of-the-mill interaction with a reviewer.
5) The novel aspect of this paper may lie in the reference to that novel vegan touchstone, Neu5Gc. Pro-tip - if the vegan diet had a magic mechanism, you ought to know it already; some major low-carb mechanisms have been understood for generations. At this rate, if there is a magic mechanism for vegan health benefit, it will be discovered by a low-carb scientist.
We now know that these food choices and their impact are at least partially precipitated by the inflammatory effect of our diets based given our inability to convert Neu5Ac to Neu5Gc and our bodies immune response to the Neu5Gc present in animal protein.
At this point, let's take the study at face value. the vegan diet avoided animal protein and Neu5Gc, the low carb diet probably included twice as much protein as the other diets (based on reference 6), but the low fat diet included more animal protein and Neu5Gc than the vegan diet.
One‐year lowered‐carbohydrate diet significantly increases cardiovascular risks, while a low‐to‐moderate‐fat diet significantly reduces cardiovascular risk factors. Vegan diets were intermediate.
So Fleming's own study, taken at face value, doesn't support the Neu5Gc hypothesis. In fact, it's unusual for the vegan diet to be inferior to the low-fat diet in any vegan study, and it's unusual for the low carb diet to be inferior to the low-fat diet in any low-carb study.
6) adherence to diets over 12 months was 100%. Of course, this is unheard of and entirely implausible; if honestly reported, it seems to show considerable gullibility or self-deception in the study team.
That 100% of participants continued on their respective diet plans through a full year of dieting contrasts sharply with much of diet research experience with drop outs and with common experience with difficulties of dieting and remaining on diets. This success can be attributed to attention to well-established psychological principles of habit acquisition and extinction and of behaviour modification through Bandura [17] counseling.
7) the original report of the 2002 study (ref 6), if it is the same study, reports diet groups differently.

8) Implausible randomisation was the red flag that saw the PREDIMED study and many others retracted. Here randomisation of n=120 into 6 groups produced this result:
The 58 female and 62 male participants were randomly assigned to equal dietary groups by casting a die. There were no statistical demographic differences between group assignments. There were no statistically significant differences, or even trends, between diet groups at the initiation of the study. Since the groups were unequivocally randomized for all fifteen-baseline indices, statistical inference to the initial population, described by Table 1, is appropriate.
9) Fleming et al state "A four-month post-intervention analysis was obtained to determine post-intervention treatment, which has not previously been reported in the literature."
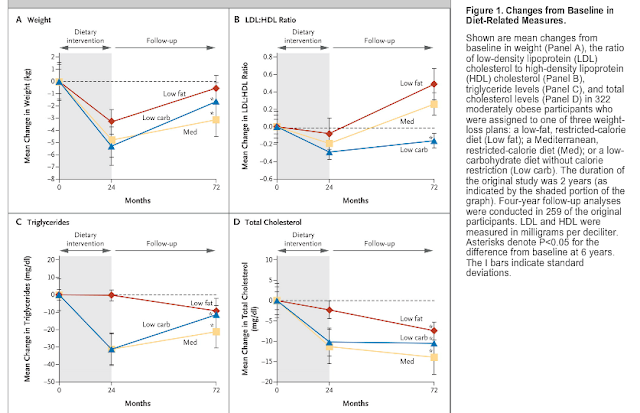
Post intervention status was in fact reported at 4 years by the Shai et al DIRECT study group.
10) the sponsor is listed as the Camelot Foundation. A search turned up this mention - Dr Fleming is the editor of a predatory journal, and the Camelot Foundation has little other existence online, it seems to be a 501(c)(3) legal tax-avoidance scheme within Fleming's own business.
https://www.omicsonline.org/editor-profile/richard-maximus-fleming/
11) Cardiovascular improvement by Fleming's medical imaging method correlates with improvement in the TG/HDL ratio. Taken at face value, although TG/HDL doesn't improve in Fleming's "low carb" arm, it does in most of the people reading this who have tried a low carb approach, so if Fleming's diagnostics are accurate this is not bad news. Interleukin 6 also improves during fasting but not a ketogenic diet in a 6-day study, but improves in a low carb diet vs a low fat diet in a 6 month study here (as there was at least one previous study in the literature that came to different conclusions from Fleming et al with regard to an outcome they highlighted, this should really have been cited).
Both LFD and LCD led to similar reductions in body weight, while beneficial effects on glycaemic control were observed in the LCD group only. After 6 months, the levels of IL-1Ra and IL-6 were significantly lower in the LCD group than in the LFD group, 978 (664–1385) versus 1216 (974–1822) pg/mL and 2.15 (1.65–4.27) versus 3.39 (2.25–4.79) pg/mL, both P < 0.05.
Taken at face value, Fleming's possibly fraudulent paper predicts cardiovascular benefit from a low carb diet if people get different results from the ones he claims to have produced, which is usually the case in other studies and in real life...
The question is, how did this paper pass peer review with all the red flags above? [edit]
Credit to @MacroFour and Ivor Cummins @FatEmperor for the links regarding Dr Fleming's colourful past.
